Leucine
 Skeletal formula of L-leucine
| |||
| |||
| Names | |||
|---|---|---|---|
| IUPAC name
Leucine
| |||
| Other names
2-Amino-4-methylpentanoic acid
| |||
| Identifiers | |||
3D model (JSmol)
|
|||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
| ECHA InfoCard | 100.000.475 | ||
| KEGG | |||
PubChem CID
|
|||
| UNII | |||
CompTox Dashboard (EPA)
|
|||
| |||
| |||
| Properties | |||
| C6H13NO2 | |||
| Molar mass | 131.175 g·mol−1 | ||
| Acidity (pKa) | 2.36 (carboxyl), 9.60 (amino)[2] | ||
| -84.9·10−6 cm3/mol | |||
| Supplementary data page | |||
| Leucine (data page) | |||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |||
Leucine (symbol Leu or L)[3] is an essential amino acid that is used in the biosynthesis of proteins. Leucine is an α-amino acid, meaning it contains an α-amino group (which is in the protonated −NH3+ form under biological conditions), an α-carboxylic acid group (which is in the deprotonated −COO− form under biological conditions), and a side chain isobutyl group, making it a non-polar aliphatic amino acid. It is essential in humans, meaning the body cannot synthesize it: it must be obtained from the diet. Human dietary sources are foods that contain protein, such as meats, dairy products, soy products, and beans and other legumes. It is encoded by the codons UUA, UUG, CUU, CUC, CUA, and CUG. Leucine is named after the Greek word for "white": λευκός (leukós, "white"), after its common appearance as a white powder, a property it shares with many other amino acids.[4]
Like valine and isoleucine, leucine is a branched-chain amino acid. The primary metabolic end products of leucine metabolism are acetyl-CoA and acetoacetate; consequently, it is one of the two exclusively ketogenic amino acids, with lysine being the other.[5] It is the most important ketogenic amino acid in humans.[6]
Leucine and β-hydroxy β-methylbutyric acid, a minor leucine metabolite, exhibit pharmacological activity in humans and have been demonstrated to promote protein biosynthesis via the phosphorylation of the mechanistic target of rapamycin (mTOR).[7][8]
Dietary leucine
[edit]As a food additive, L-leucine has E number E641 and is classified as a flavor enhancer.[9]
Requirements
[edit]The Food and Nutrition Board (FNB) of the U.S. Institute of Medicine set Recommended Dietary Allowances (RDAs) for essential amino acids in 2002. For leucine, for adults 19 years and older, 42 mg/kg body weight/day.[10]
Sources
[edit]| Food | g/100g |
|---|---|
| Whey protein concentrate, dry powder | 10.0–12.0 |
| Soy protein concentrate, dry powder | 7.5–8.5 |
| Pea protein concentrate, dry powder | 6.6 |
| Soybeans, mature seeds, roasted, salted | 2.87 |
| Hemp seed, hulled | 2.16 |
| Beef, round, top round, raw | 1.76 |
| Peanuts | 1.67 |
| Fish, salmon, pink, raw | 1.62 |
| Wheat germ | 1.57 |
| Almonds | 1.49 |
| Chicken, broilers or fryers, thigh, raw | 1.48 |
| Chicken egg, yolk, raw | 1.40 |
| Oats | 1.28 |
| Edamame (soybeans, green, raw) | 0.93 |
| Beans, pinto, cooked | 0.78 |
| Lentils, cooked | 0.65 |
| Chickpea, cooked | 0.63 |
| Corn, yellow | 0.35 |
| Cow milk, whole, 3.25% milk fat | 0.27 |
| Rice, brown, medium-grain, cooked | 0.19 |
| Milk, human, mature, fluid | 0.10 |
Health effects
[edit]As a dietary supplement, leucine has been found to slow the degradation of muscle tissue by increasing the synthesis of muscle proteins in aged rats.[12] However, results of comparative studies are conflicted. Long-term leucine supplementation does not increase muscle mass or strength in healthy elderly men.[13] More studies are needed, preferably ones based on an objective, random sample of society. Factors such as lifestyle choices, age, gender, diet, exercise, etc. must be factored into the analyses to isolate the effects of supplemental leucine as a stand-alone, or if taken with other branched-chain amino acids (BCAAs). Until then, dietary supplemental leucine cannot be associated as the prime reason for muscular growth or optimal maintenance for the entire population.
Both L-leucine and D-leucine protect mice against epileptic seizures.[14] D-leucine also terminates seizures in mice after the onset of seizure activity, at least as effectively as diazepam and without sedative effects.[14] Decreased dietary intake of L-leucine lessens adiposity in mice.[15] High blood levels of leucine are associated with insulin resistance in humans, mice, and rodents.[16] This might be due to the effect of leucine to stimulate mTOR signaling.[17] Dietary restriction of leucine and the other BCAAs can reverse diet-induced obesity in wild-type mice by increasing energy expenditure, and can restrict fat mass gain of hyperphagic rats.[18][19]
Safety
[edit]Leucine toxicity, as seen in decompensated maple syrup urine disease, causes delirium and neurologic compromise, and can be life-threatening.[20]
A high intake of leucine may cause or exacerbate symptoms of pellagra in people with low niacin status because it interferes with the conversion of L-tryptophan to niacin.[21]
Leucine at a dose exceeding 500 mg/kg/d was observed with hyperammonemia.[22] As such, unofficially, a tolerable upper intake level (UL) for leucine in healthy adult men can be suggested at 500 mg/kg/d or 35 g/d under acute dietary conditions.[22][23]
Pharmacology
[edit]Pharmacodynamics
[edit]Leucine is a dietary amino acid with the capacity to directly stimulate myofibrillar muscle protein synthesis.[24] This effect of leucine results from its role as an activator of the mechanistic target of rapamycin (mTOR),[8] a serine-threonine protein kinase that regulates protein biosynthesis and cell growth. The activation of mTOR by leucine is mediated through Rag GTPases,[25][26][27] leucine binding to leucyl-tRNA synthetase,[25][26] leucine binding to sestrin 2,[28][29][30] and possibly other mechanisms.
Metabolism in humans
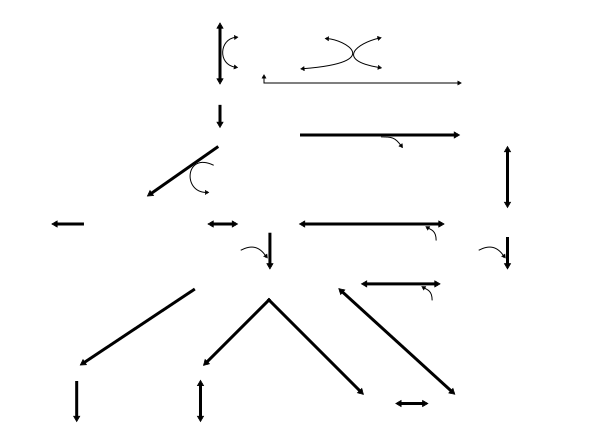
[edit]Leucine metabolism in humans
|
Leucine metabolism occurs in many tissues in the human body; however, most dietary leucine is metabolized within the liver, adipose tissue, and muscle tissue.[36] Adipose and muscle tissue use leucine in the formation of sterols and other compounds.[36] Combined leucine use in these two tissues is seven times greater than in the liver.[36]
In healthy individuals, approximately 60% of dietary L-leucine is metabolized after several hours, with roughly 5% (2–10% range) of dietary L-leucine being converted to β-hydroxy β-methylbutyric acid (HMB).[37][38][35] Around 40% of dietary L-leucine is converted to acetyl-CoA, which is subsequently used in the synthesis of other compounds.[35]
The vast majority of L-leucine metabolism is initially catalyzed by the branched-chain amino acid aminotransferase enzyme, producing α-ketoisocaproate (α-KIC).[37][35] α-KIC is mostly metabolized by the mitochondrial enzyme branched-chain α-ketoacid dehydrogenase, which converts it to isovaleryl-CoA.[37][35] Isovaleryl-CoA is subsequently metabolized by isovaleryl-CoA dehydrogenase and converted to MC-CoA, which is used in the synthesis of acetyl-CoA and other compounds.[35] During biotin deficiency, HMB can be synthesized from MC-CoA via enoyl-CoA hydratase and an unknown thioesterase enzyme,[31][32][39] which convert MC-CoA into HMB-CoA and HMB-CoA into HMB respectively.[32] A relatively small amount of α-KIC is metabolized in the liver by the cytosolic enzyme 4-hydroxyphenylpyruvate dioxygenase (KIC dioxygenase), which converts α-KIC to HMB.[37][35][40] In healthy individuals, this minor pathway – which involves the conversion of L-leucine to α-KIC and then HMB – is the predominant route of HMB synthesis.[37][35]
A small fraction of L-leucine metabolism – less than 5% in all tissues except the testes, where it accounts for about 33% – is initially catalyzed by leucine aminomutase, producing β-leucine, which is subsequently metabolized into β-ketoisocaproate (β-KIC), β-ketoisocaproyl-CoA, and then acetyl-CoA by a series of uncharacterized enzymes.[35][41]
The metabolism of HMB is catalyzed by an uncharacterized enzyme which converts it to β-hydroxy β-methylbutyryl-CoA (HMB-CoA).[31][35] HMB-CoA is metabolized by either enoyl-CoA hydratase or another uncharacterized enzyme, producing β-methylcrotonyl-CoA (MC-CoA) or hydroxymethylglutaryl-CoA (HMG-CoA) respectively.[37][35] MC-CoA is then converted by the enzyme methylcrotonyl-CoA carboxylase to methylglutaconyl-CoA (MG-CoA), which is subsequently converted to HMG-CoA by methylglutaconyl-CoA hydratase.[37][35][41] HMG-CoA is then cleaved into acetyl-CoA and acetoacetate by HMG-CoA lyase or used in the production of cholesterol via the mevalonate pathway.[37][35]
Synthesis in nonhuman organisms
[edit]Leucine is an essential amino acid in the diet of animals because they lack the complete enzyme pathway to synthesize it de novo from potential precursor compounds. Consequently, they must ingest it, usually as a component of proteins. Plants and microorganisms synthesize leucine from pyruvic acid with a series of enzymes:[42]
- Acetolactate synthase
- Acetohydroxy acid isomeroreductase
- Dihydroxyacid dehydratase
- α-Isopropylmalate synthase
- α-Isopropylmalate isomerase
- Leucine aminotransferase
Synthesis of the small, hydrophobic amino acid valine also includes the initial part of this pathway.
Chemistry
[edit]
Leucine is a branched-chain amino acid (BCAA) since it possesses an aliphatic side chain that is not linear.
Racemic leucine had been[when?] subjected to circularly polarized synchrotron radiation to better understand the origin of biomolecular asymmetry. An enantiomeric enhancement of 2.6% had been induced, indicating a possible photochemical origin of biomolecules' homochirality.[43]
See also
[edit]- Leucines, the isomers and derivatives of leucine
- Leucine zipper, a common motif in transcription factor proteins
Notes
[edit]- ^ This reaction is catalyzed by an unknown thioesterase enzyme.[31][32]
References
[edit]- ^ a b Binns J, Parsons S, McIntyre GJ (December 2016). "Accurate hydrogen parameters for the amino acid L-leucine" (PDF). Acta Crystallographica Section B. 72 (Pt 6): 885–92. doi:10.1107/S2052520616015699. hdl:20.500.11820/c784fdaf-aa3a-48e4-86a2-d0a0bd7fdb7a. PMID 27910839. S2CID 19288938.
- ^ Dawson, R.M.C., et al., Data for Biochemical Research, Oxford, Clarendon Press, 1959.
- ^ "Nomenclature and Symbolism for Amino Acids and Peptides". IUPAC-IUB Joint Commission on Biochemical Nomenclature. 1983. Archived from the original on 9 October 2008. Retrieved 5 March 2018.
- ^ Fleck, Michel; Petrosyan, Aram M. (2014). Salts of Amino Acids: Crystallization, Structure and Properties. Cham: Springer International Publishing. doi:10.1007/978-3-319-06299-0. ISBN 978-3-319-06298-3.
- ^ Ferrier DR (2013). Biochemistry. Lippincott Williams & Wilkins. ISBN 9781451175622.
- ^ Cynober LA (2003). Metabolic & Therapeutic Aspects of Amino Acids in Clinical Nutrition (2nd ed.). CRC Press. p. 101. ISBN 9780203010266.
- ^ Silva VR, Belozo FL, Micheletti TO, Conrado M, Stout JR, Pimentel GD, Gonzalez AM (September 2017). "β-hydroxy-β-methylbutyrate free acid supplementation may improve recovery and muscle adaptations after resistance training: a systematic review". Nutrition Research. 45: 1–9. doi:10.1016/j.nutres.2017.07.008. hdl:11449/170023. PMID 29037326.
HMB's mechanisms of action are generally considered to relate to its effect on both muscle protein synthesis and muscle protein breakdown (Figure 1) [2, 3]. HMB appears to stimulate muscle protein synthesis through an up-regulation of the mammalian/mechanistic target of rapamycin complex 1 (mTORC1), a signaling cascade involved in coordination of translation initiation of muscle protein synthesis [2, 4]. Additionally, HMB may have antagonistic effects on the ubiquitin–proteasome pathway, a system that degrades intracellular proteins [5, 6]. Evidence also suggests that HMB promotes myogenic proliferation, differentiation, and cell fusion [7]. ... Exogenous HMB-FA administration has shown to increase intramuscular anabolic signaling, stimulate muscle protein synthesis, and attenuate muscle protein breakdown in humans [2].
- ^ a b Wilkinson DJ, Hossain T, Hill DS, Phillips BE, Crossland H, Williams J, et al. (June 2013). "Effects of leucine and its metabolite β-hydroxy-β-methylbutyrate on human skeletal muscle protein metabolism". The Journal of Physiology. 591 (11): 2911–23. doi:10.1113/jphysiol.2013.253203. PMC 3690694. PMID 23551944.
The stimulation of MPS through mTORc1-signalling following HMB exposure is in agreement with pre-clinical studies (Eley et al. 2008). ... Furthermore, there was clear divergence in the amplitude of phosphorylation for 4EBP1 (at Thr37/46 and Ser65/Thr70) and p70S6K (Thr389) in response to both Leu and HMB, with the latter showing more pronounced and sustained phosphorylation. ... Nonetheless, as the overall MPS response was similar, this cellular signalling distinction did not translate into statistically distinguishable anabolic effects in our primary outcome measure of MPS. ... Interestingly, although orally supplied HMB produced no increase in plasma insulin, it caused a depression in MPB (−57%). Normally, postprandial decreases in MPB (of ~50%) are attributed to the nitrogen-sparing effects of insulin since clamping insulin at post-absorptive concentrations (5 μU ml−1) while continuously infusing AAs (18 g h−1) did not suppress MPB (Greenhaff et al. 2008), which is why we chose not to measure MPB in the Leu group, due to an anticipated hyperinsulinaemia (Fig. 3C). Thus, HMB reduces MPB in a fashion similar to, but independent of, insulin. These findings are in-line with reports of the anti-catabolic effects of HMB suppressing MPB in pre-clinical models, via attenuating proteasomal-mediated proteolysis in response to LPS (Eley et al. 2008).
- ^ Winter R (2009). A consumer's dictionary of food additives (7th ed.). New York: Three Rivers Press. ISBN 978-0307408921.
- ^ Institute of Medicine (2002). "Protein and Amino Acids". Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: The National Academies Press. pp. 589–768. doi:10.17226/10490. ISBN 978-0-309-08525-0.
- ^ National Nutrient Database for Standard Reference. U.S. Department of Agriculture. Archived from the original on 3 March 2015. Retrieved 16 September 2009.
- ^ Combaret L, Dardevet D, Rieu I, Pouch MN, Béchet D, Taillandier D, et al. (December 2005). "A leucine-supplemented diet restores the defective postprandial inhibition of proteasome-dependent proteolysis in aged rat skeletal muscle". The Journal of Physiology. 569 (Pt 2): 489–99. doi:10.1113/jphysiol.2005.098004. PMC 1464228. PMID 16195315.
- ^ Verhoeven S, Vanschoonbeek K, Verdijk LB, Koopman R, Wodzig WK, Dendale P, van Loon LJ (May 2009). "Long-term leucine supplementation does not increase muscle mass or strength in healthy elderly men". The American Journal of Clinical Nutrition. 89 (5): 1468–75. doi:10.3945/ajcn.2008.26668. PMID 19321567.
- ^ a b Hartman AL, Santos P, O'Riordan KJ, Stafstrom CE, Marie Hardwick J (October 2015). "Potent anti-seizure effects of D-leucine". Neurobiology of Disease. 82: 46–53. doi:10.1016/j.nbd.2015.05.013. PMC 4640989. PMID 26054437.
- ^ Fontana L, Cummings NE, Arriola Apelo SI, Neuman JC, Kasza I, Schmidt BA, et al. (July 2016). "Decreased Consumption of Branched-Chain Amino Acids Improves Metabolic Health". Cell Reports. 16 (2): 520–30. doi:10.1016/j.celrep.2016.05.092. PMC 4947548. PMID 27346343.
- ^ Lynch CJ, Adams SH (December 2014). "Branched-chain amino acids in metabolic signalling and insulin resistance". Nature Reviews. Endocrinology. 10 (12): 723–36. doi:10.1038/nrendo.2014.171. PMC 4424797. PMID 25287287.
- ^ Caron A, Richard D, Laplante M (2015). "The Roles of mTOR Complexes in Lipid Metabolism". Annual Review of Nutrition. 35: 321–48. doi:10.1146/annurev-nutr-071714-034355. PMID 26185979.
- ^ Cummings NE, Williams EM, Kasza I, Konon EN, Schaid MD, Schmidt BA, et al. (February 2018). "Restoration of metabolic health by decreased consumption of branched-chain amino acids". The Journal of Physiology. 596 (4): 623–45. doi:10.1113/JP275075. PMC 5813603. PMID 29266268.
- ^ White PJ, Lapworth AL, An J, Wang L, McGarrah RW, Stevens RD, et al. (July 2016). "Branched-chain amino acid restriction in Zucker-fatty rats improves muscle insulin sensitivity by enhancing efficiency of fatty acid oxidation and acyl-glycine export". Molecular Metabolism. 5 (7): 538–51. doi:10.1016/j.molmet.2016.04.006. PMC 4921791. PMID 27408778.
- ^ Yudkoff, Marc; Daikhin, Yevgeny; Nissim, Ilana; Horyn, Oksana; Luhovyy, Bohdan; Lazarow, Adam; Nissim, Itzhak (1 June 2005). "Brain Amino Acid Requirements and Toxicity: The Example of Leucine". The Journal of Nutrition. 135 (6): 1531S – 38S. doi:10.1093/jn/135.6.1531S. ISSN 0022-3166. PMID 15930465.
- ^ Badawy AA, Lake SL, Dougherty DM (2014). "Mechanisms of the pellagragenic effect of leucine: stimulation of hepatic tryptophan oxidation by administration of branched-chain amino acids to healthy human volunteers and the role of plasma free tryptophan and total kynurenines". International Journal of Tryptophan Research. 7: 23–32. doi:10.4137/IJTR.S18231. PMC 4259507. PMID 25520560.
- ^ a b Elango R, Chapman K, Rafii M, Ball RO, Pencharz PB (October 2012). "Determination of the tolerable upper intake level of leucine in acute dietary studies in young men". The American Journal of Clinical Nutrition. 96 (4): 759–67. doi:10.3945/ajcn.111.024471. PMID 22952178.
A significant increase in blood ammonia concentrations above normal values, plasma leucine concentrations, and urinary leucine excretion were observed with leucine intakes >500 mg · kg−1 · d−1. The oxidation of l-[1-13C]-leucine expressed as label tracer oxidation in breath (F13CO2), leucine oxidation, and α-ketoisocaproic acid (KIC) oxidation led to different results: a plateau in F13CO2 observed after 500 mg · kg−1 · d−1, no clear plateau observed in leucine oxidation, and KIC oxidation appearing to plateau after 750 mg · kg−1 · d−1. On the basis of plasma and urinary variables, the UL for leucine in healthy adult men can be suggested at 500 mg · kg−1 · d−1 or ~35 g/d as a cautious estimate under acute dietary conditions.
- ^ Rasmussen B, Gilbert E, Turki A, Madden K, Elango R (July 2016). "Determination of the safety of leucine supplementation in healthy elderly men". Amino Acids. 48 (7): 1707–16. doi:10.1007/s00726-016-2241-0. PMID 27138628. S2CID 3708265.
the upper limit for leucine intake in healthy elderly could be set similar to young men at 500 mg kg-1 day-1 or ~35 g/day for an individual weighing 70 kg
- ^ Etzel MR (April 2004). "Manufacture and use of dairy protein fractions". The Journal of Nutrition. 134 (4): 996S – 1002S. doi:10.1093/jn/134.4.996S. PMID 15051860.
- ^ a b Kim JH, Lee C, Lee M, Wang H, Kim K, Park SJ, et al. (September 2017). "Control of leucine-dependent mTORC1 pathway through chemical intervention of leucyl-tRNA synthetase and RagD interaction". Nature Communications. 8 (1): 732. Bibcode:2017NatCo...8..732K. doi:10.1038/s41467-017-00785-0. PMC 5622079. PMID 28963468.
- ^ a b Jewell JL, Russell RC, Guan KL (March 2013). "Amino acid signalling upstream of mTOR". Nature Reviews. Molecular Cell Biology. 14 (3): 133–39. doi:10.1038/nrm3522. PMC 3988467. PMID 23361334.
- ^ Sancak Y, Peterson TR, Shaul YD, Lindquist RA, Thoreen CC, Bar-Peled L, Sabatini DM (June 2008). "The Rag GTPases bind raptor and mediate amino acid signaling to mTORC1". Science. 320 (5882): 1496–501. Bibcode:2008Sci...320.1496S. doi:10.1126/science.1157535. PMC 2475333. PMID 18497260.
- ^ Wolfson RL, Chantranupong L, Saxton RA, Shen K, Scaria SM, Cantor JR, Sabatini DM (January 2016). "Sestrin2 is a leucine sensor for the mTORC1 pathway". Science. 351 (6268): 43–48. Bibcode:2016Sci...351...43W. doi:10.1126/science.aab2674. PMC 4698017. PMID 26449471.
- ^ Saxton RA, Knockenhauer KE, Wolfson RL, Chantranupong L, Pacold ME, Wang T, et al. (January 2016). "Structural basis for leucine sensing by the Sestrin2-mTORC1 pathway". Science. 351 (6268): 53–58. Bibcode:2016Sci...351...53S. doi:10.1126/science.aad2087. PMC 4698039. PMID 26586190.
- ^ Chantranupong L, Wolfson RL, Orozco JM, Saxton RA, Scaria SM, Bar-Peled L, et al. (October 2014). "The Sestrins interact with GATOR2 to negatively regulate the amino-acid-sensing pathway upstream of mTORC1". Cell Reports. 9 (1): 1–8. doi:10.1016/j.celrep.2014.09.014. PMC 4223866. PMID 25263562.
- ^ a b c "KEGG Reaction: R10759". Kyoto Encyclopedia of Genes and Genomes. Kanehisa Laboratories. Archived from the original on 1 July 2016. Retrieved 24 June 2016.
- ^ a b c Mock DM, Stratton SL, Horvath TD, Bogusiewicz A, Matthews NI, Henrich CL, Dawson AM, Spencer HJ, Owen SN, Boysen G, Moran JH (November 2011). "Urinary excretion of 3-hydroxyisovaleric acid and 3-hydroxyisovaleryl carnitine increases in response to a leucine challenge in marginally biotin-deficient humans". primary source. The Journal of Nutrition. 141 (11): 1925–1930. doi:10.3945/jn.111.146126. PMC 3192457. PMID 21918059.
Reduced activity of MCC impairs catalysis of an essential step in the mitochondrial catabolism of the BCAA leucine. Metabolic impairment diverts methylcrotonyl CoA to 3-hydroxyisovaleryl CoA in a reaction catalyzed by enoyl-CoA hydratase (22, 23). 3-Hydroxyisovaleryl CoA accumulation can inhibit cellular respiration either directly or via effects on the ratios of acyl CoA:free CoA if further metabolism and detoxification of 3-hydroxyisovaleryl CoA does not occur (22). The transfer to carnitine by 4 carnitine acyl-CoA transferases distributed in subcellular compartments likely serves as an important reservoir for acyl moieties (39–41). 3-Hydroxyisovaleryl CoA is likely detoxified by carnitine acetyltransferase producing 3HIA-carnitine, which is transported across the inner mitochondrial membrane (and hence effectively out of the mitochondria) via carnitine-acylcarnitine translocase (39). 3HIA-carnitine is thought to be either directly deacylated by a hydrolase to 3HIA or to undergo a second CoA exchange to again form 3-hydroxyisovaleryl CoA followed by release of 3HIA and free CoA by a thioesterase.
- ^ a b Wilson JM, Fitschen PJ, Campbell B, Wilson GJ, Zanchi N, Taylor L, Wilborn C, Kalman DS, Stout JR, Hoffman JR, Ziegenfuss TN, Lopez HL, Kreider RB, Smith-Ryan AE, Antonio J (February 2013). "International Society of Sports Nutrition Position Stand: beta-hydroxy-beta-methylbutyrate (HMB)". Journal of the International Society of Sports Nutrition. 10 (1): 6. doi:10.1186/1550-2783-10-6. PMC 3568064. PMID 23374455.
- ^ a b c d e f g h i j k l m n Kohlmeier M (May 2015). "Leucine". Nutrient Metabolism: Structures, Functions, and Genes (2nd ed.). Academic Press. pp. 385–388. ISBN 978-0-12-387784-0. Archived from the original on 22 March 2018. Retrieved 6 June 2016.
Energy fuel: Eventually, most Leu is broken down, providing about 6.0kcal/g. About 60% of ingested Leu is oxidized within a few hours ... Ketogenesis: A significant proportion (40% of an ingested dose) is converted into acetyl-CoA and thereby contributes to the synthesis of ketones, steroids, fatty acids, and other compounds
Figure 8.57: Metabolism of L-leucine Archived 22 March 2018 at the Wayback Machine - ^ a b c Rosenthal J, Angel A, Farkas J (February 1974). "Metabolic fate of leucine: a significant sterol precursor in adipose tissue and muscle". The American Journal of Physiology. 226 (2): 411–18. doi:10.1152/ajplegacy.1974.226.2.411. PMID 4855772.
- ^ Brioche T, Pagano AF, Py G, Chopard A (August 2016). "Muscle wasting and aging: Experimental models, fatty infiltrations, and prevention" (PDF). Molecular Aspects of Medicine. 50: 56–87. doi:10.1016/j.mam.2016.04.006. PMID 27106402. S2CID 29717535.
In conclusion, HMB treatment clearly appears to be a safe potent strategy against sarcopenia, and more generally against muscle wasting, because HMB improves muscle mass, muscle strength, and physical performance. It seems that HMB is able to act on three of the four major mechanisms involved in muscle deconditioning (protein turnover, apoptosis, and the regenerative process), whereas it is hypothesized to strongly affect the fourth (mitochondrial dynamics and functions). Moreover, HMB is inexpensive (~30– 50 US dollars per month at 3 g per day) and may prevent osteopenia (Bruckbauer and Zemel, 2013; Tatara, 2009; Tatara et al., 2007, 2008, 2012) and decrease cardiovascular risks (Nissen et al., 2000). For all these reasons, HMB should be routinely used in muscle-wasting conditions especially in aged people. ... 3 g of CaHMB taken three times a day (1 g each time) is the optimal posology, which allows for continual bioavailability of HMB in the body (Wilson et al., 2013)
- ^ "KEGG Reaction: R04137". Kyoto Encyclopedia of Genes and Genomes. Kanehisa Laboratories. Archived from the original on 1 July 2016. Retrieved 24 June 2016.
- ^ "Homo sapiens: 4-hydroxyphenylpyruvate dioxygenase reaction". MetaCyc. SRI International. 20 August 2012. Retrieved 6 June 2016.
- ^ a b "Leucine metabolism". BRENDA. Technische Universität Braunschweig. Archived from the original on 17 August 2016. Retrieved 12 August 2016.
- ^ Lehninger AL, Nelson DL, Cox MM (2000). Lehninger principles of biochemistry (3rd ed.). New York: Worth Publishers. ISBN 978-1-57259-153-0.
- ^ Meierhenrich: Amino acids and the asymmetry of life, Springer-Verlag, 2008, ISBN 978-3-540-76885-2.
External links
[edit]- Leucine Biosynthesis at the Wayback Machine (archived 2017-05-06)